Why is this claim secondary claim unbalanced
Secondary Claim Unbalanced
There are several reasons why a claim can be considered unbalanced.
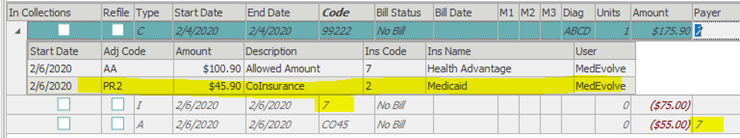
- The insurance payment, adjustment, and/or allowed amount and patient responsibility is off. You can make sure the numbers balance by using the following equation. If you are going off the EOB or the remittance was auto posted the math should already be correct.
- Charge amount - Adjustment = Allowed Amount
- Allowed Amount - Insurance Payment = Patient Responsibility
- The claim was not adjudicated before it left the MedEvolve system.
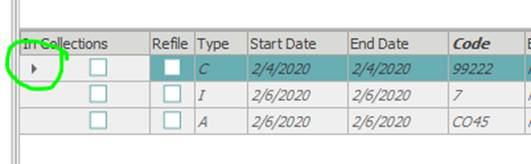
- There is no COB information on the transaction. The COB information is shown as a black triangle next to the charge.
- The insurance plan selected in the COB information is the secondary plan and not the primary plan.
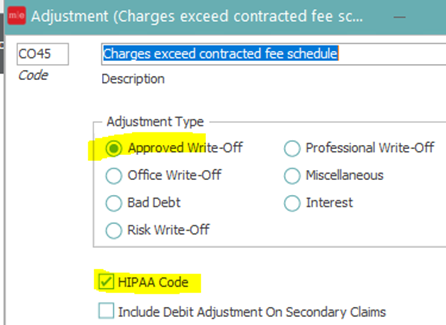
- The adjustment code is not flagged as approved write off and/or HIPPA compliant code in the adjustment table.
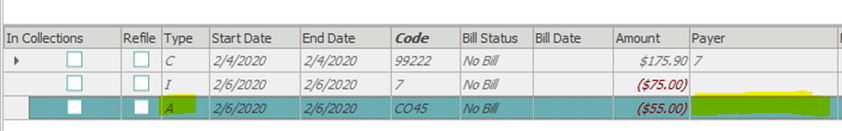
- There is no payer attached to the adjustment line.
- There is duplicate information in the COB tab.
- You are only allowed one of each code AA, PR1, PR2, and PR3.
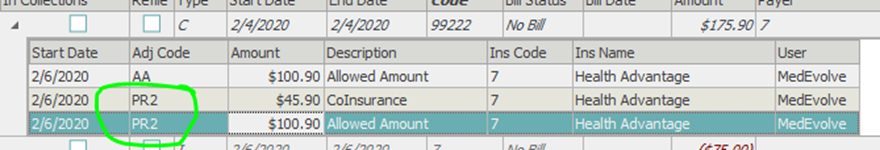
- You are only allowed one of each code AA, PR1, PR2, and PR3.
- There is an adjustment code in the COB tab.
Adjustment codes should never be posted in the COB information. They should only be posted as an adjustment line.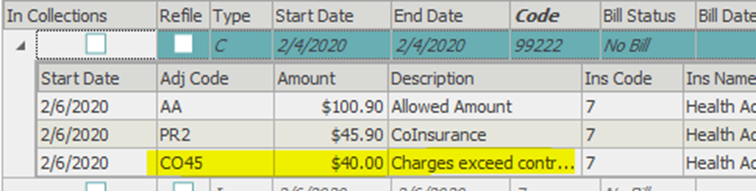
These are just a few examples of things that could make a claim fall on the Unprocessable Claims Report for Secondary Claims Unbalanced. If you have checked all of these and do not see an issue and require further assistance please open a case with support. Reach out at support@medevolve.com or call 1-800-964-5129 option 1.
