Why am I receiving a rejection for Entitys claim filing indicator?
Entitys Claim Filing Indicator Rejection
Within Practice Insight claims can be rejected with the following message, "A7:480 Acknowledgement/Rejected for Invalid Information - The claim/encounter has invalid information as specified in the Status details and has been rejected. Entitys claim filing indicator. Usage: This code requires use of an Entity Code.: Entity Payer (A7:480: PR)"
The key phrase is Entity claim filing indicator. This will occur when two insurance plans are setup with the claim filing indicator MB (Medicare Part B). Should a claim have traditional Medicare and DMERC, or traditional Medicare and Medicare replacement plan also attached to the Medicare category, this rejection will pop up on the rejection listing.
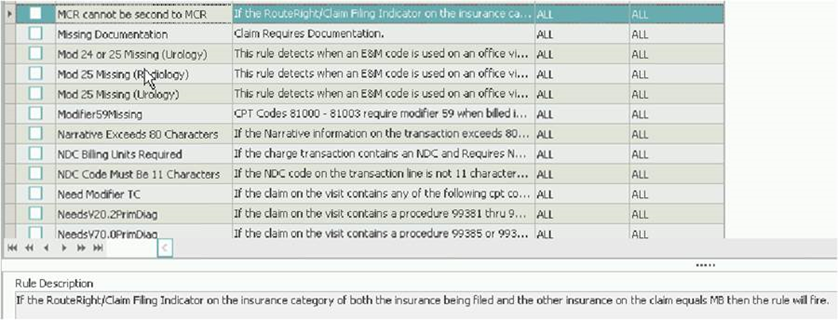
To stop claims from processing from Medevolve to Practice Insight, a claim rule is available to process these claims to the Unprocessable Claims Report until corrected.
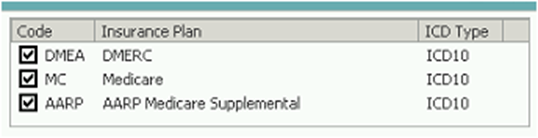
MCR cannot be second to MCR - this will need to be set for the categories: DMERC, Medicare and Railroad Medicare.
On the patient's visit, unselect traditional Medicare before refiling the claim, or the Unprocessable Claims Report able to release for claim submission to Practice Insight.