PM 8.1.25.0 Release Notes
What's new and what's fixed in November 2023
What’s New?
Eligibility Enhancements
New status color for ‘Other Insurance’
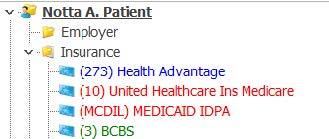
A new Eligibility status color has been added to indicate that coverage is active, but with another payer. We are now coloring the insurance plan name in blue font, if the status is returned ‘Inactive: Other Insurance’. This will alert users that something needs to be addressed. Currently this status is only returned for Medicare and Blue Cross / Blue Shield plans.
Posting Enhancements
Several new feature options have been added in the Posting module to aid in automating processes and allow users to work more effectively.
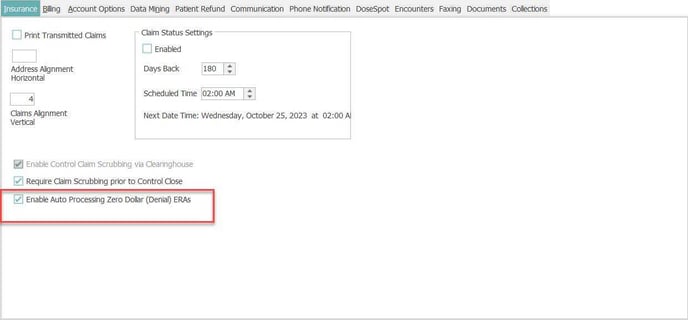
Auto-Process Denial ERAs
A new option to have Remittances that contain all denials, no payments, to auto-process upon receipt has been added. To enable this option, go to Enterprise Manager under the Insurance tab and check the option ‘Enable auto Processing Zero Dollar (Denial) ERAs’.
Since these ERAs have no payments or adjustments to process, this option simply marks the ERA as ‘Processed’, allowing it to be removed from the list of ERAs under the Remittance tab. All the actionable denial information will be linked to the claims in order to work the claims via Insurance Collections and Workflow.
Posting inbound queue Enhancements
We are now considering the users posting preferences when processing transactions from the inbound queue. If visit data is missing from the queue and the user has preferences set to default data points from the patient’s previous visit, when the visit is created will default any data points configured by the user from the patient’s previous visit to the newly created visit, alleviating the need for the user to manually input.
Auto-process option for DEPOSIT
A new option has been added to auto-link a charge transaction to a DEPOSIT payment when processing the charge from the queue into a control. To auto-link the date of service on the charge must match the date on the DEPOSIT. Just like the option to auto-link an UNAPP payment, the charge matching the DEPOSIT date of service, will replace the DEPOSIT charge and the payment will be linked to the new charge. If both a UNAPP and a DEPOSIT exist for the patient with the same date of service and both auto-link options are enabled, the auto-link will be made to the UNAPP.
To enable this functionality, contact your MedEvolve PM Support team at Support@MedEvolve.com
Option to auto-process adjustment and Payments
MedEvolve posting inbound queue can now process incoming insurance payment and adjustment transactions from a 3rd party source.
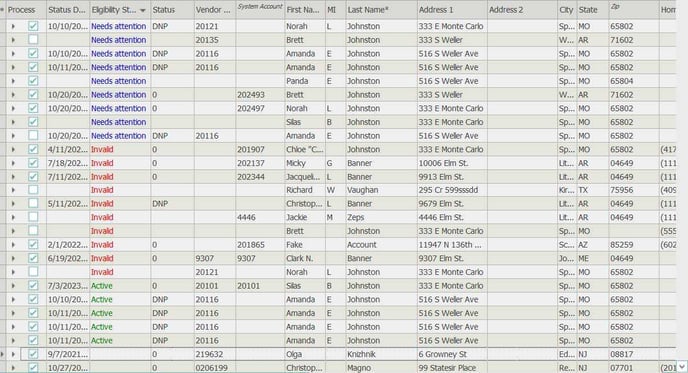
Account Queue
To expedite the review and processing of inbound demographic and patient insurance information, we are now attempting to auto-link the patients’ incoming insurance plan name to the most likely match of an existing plan code from the Insurance Table. This solution would remove the manual work of a user selecting, searching and then making the match themselves.
We first attempt to match the name received to an exact match of plan name in tables. If this cannot be done, we then attempt to match based on the 1st 5 characters of the plan name received to a plan in tables that contains those 5 characters.
After the match is made, an automated eligibility inquiry is run to verify if the auto-matching performed was accurate. If the inquiry returns a successful eligibility verification, then nothing else needs to occur with that record. If, instead, a negative verification comes back, the system will automatically remove that matched payer plan, make a 2nd match attempt and re-run eligibility. This process will continue until a successful status is returned or after the 5th attempt to match has failed.
In addition, we have added a new column to the patient demographic information to display the eligibility status results, so the user can review these at a glance without having to expand the insurance sub-grid.
If all insurance records for the account are returned active – the status will show as active
If all records are inactive – The status will show as invalid
If any combo of active, inactive: Other Insurance, inactive, failed, or blank, the status will show as needs attention
If no records have a status – this field will be blank
Scheduler
We have improved the hover hint feature within the scheduler. It no longer requires a user to click within the appointment slot to display the hover hint. If a user brings focus over the appointment slot, the hover hint will display and if the focus is moved, the hint will be removed.
Scheduler MedMat
In addition to the overall scheduler fill rate displayed at the top of the MedMat, we have added a fill rate percentage to grid when grouped by either Service Provider, Service Location, Appointment Category, Reason or Status.
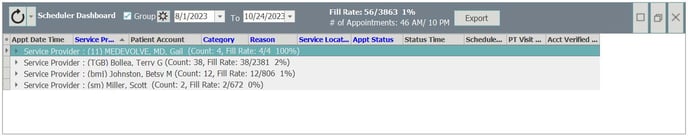
An export option has been added as well, allowing user to export the results on the Dashboard in an Excel format.
Reports
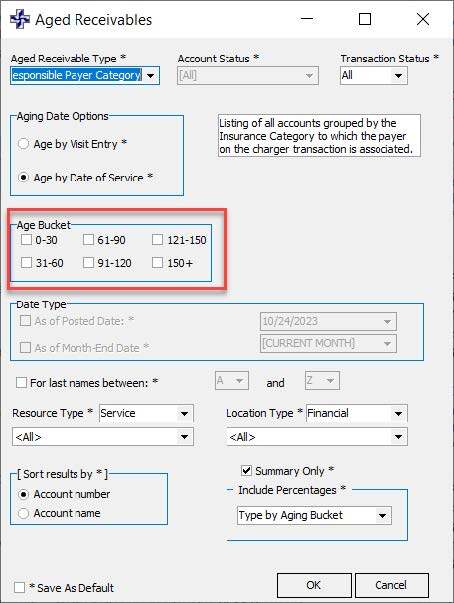
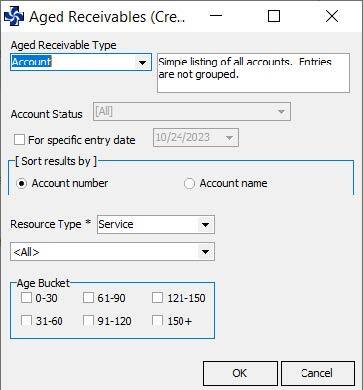
Additional parameter options have been added to both the Aged Receivables report and the Aged Receivables (credit) report.
Aged Receivables
Users can now filter the results of the AR report by aging buckets
Aged Receivables (Credit)
New parameter options to filter the results by provider, as well as by Aging buckets have been added.
Encryption
Encryption has been added for data communication between the Data and Media services and the application.
What’s fixed
Account Information
- Fixed issue that produced an erroneous warning regarding possible duplicate accounts when adding a new account with no SSN
- Now properly reflecting the correct font color for patient insurance plans based on eligibility results
Claim History
- Now displaying the custom claim rule description as well as the name of the rule when the claim is Unprocessable
Custom Claim Rules
- Fixed issue preventing a Custom Claim Rule from being saved when no filter sets existed, to correct UCR Incorrect Syntax near the Keyword 'CASE' error
Eligibility
- Unable to insert a new eligibility configuration schedule if one does not exist
- Eligibility requests from the patient tree and account queue are resulting in user getting an error 'Error Processing Eligibility Request' but after dismissing the error, the process does run.
- Fixed issue causing instances where Eligibility responses are not updating the font color of the insurance w/in the Patient Tree
Patient Messaging
- Fixed issue causing some patient responses not to display properly in message history
- Appointment Follow Up Messages need to adhere to the correct configuration & only send follow ups for the desired days out
- Appointment Reminders: Multiple days out - SP appears to be adding all days together to determine when to notify patients
Posting
- Now adhering to the requirement flags set on Insurance plans when saving a visit
- Fixed an issue that was causing transactions to be set to a ‘Bill’ status but with no Bill date
- Fixed issue in Line Posting when tabbing out of the claim key field, the visits and transactions grids are disabled and are not re-enabled when claim key is removed
Scheduler
- Updated hover hint to enable when mouse wheels over appointment slot and disables when mouse is removed
- Fixed eligibility status color for patient insurance. Now properly updating the font color (red/green/blue) of the insurance & co-pay
- Now when ePayments from the scheduler and the client’s Instamed Account is set up by Financial Location, the financial location entry on the payment form will be required.
- Fixed error presented when attempting to save an appointment template name longer than 15 characters
- Add performance improvements when loading scheduler
Scheduler MedMat
- Fixed issue with Fill rate when viewing future appointment date ranges.
- Fixed issue that was causing incorrect provider information to print on documents when generated from the MedMat
- PT Visit Count is now displaying the correct count from the Scheduler MedMat.
General
- Fixed issue that was causing the application significantly longer to load at log-in in
