Practice Management Out-of-the-Box Reports
View and analysis pre-prepared reports in practice management
From the homepage in MedEvolve, click Report.
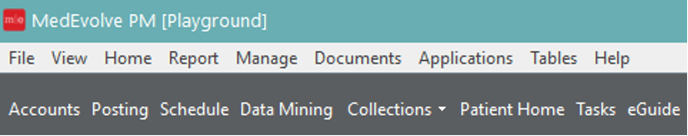
Select Create Report
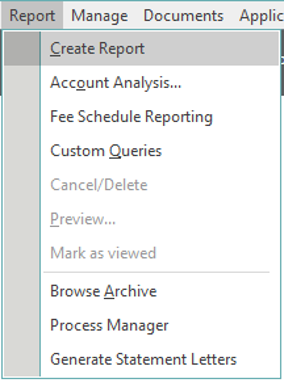
A separate screen will open
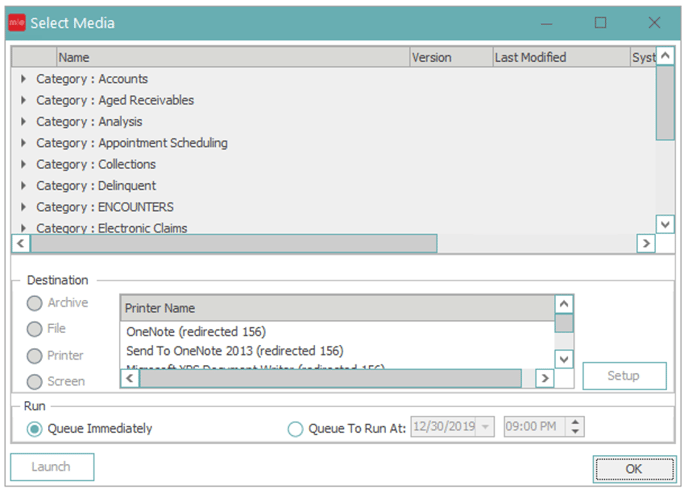
Select the drop down arrow next to the category of the report you want to run
Click the report that you want to run and choose the desired destination: Archive, Printer or Screen.

Click OK
![]()
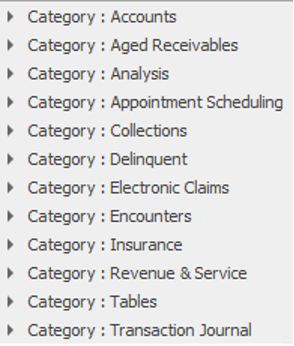
Accounts
Account Reminders → will display 'Printed' reminders that have been setup on patient accounts.
Account Recalls → will list recalls for a specified date range.
Envelope → will generate an envelope for the current Account.
Deposit Report → will list all types of payments (both insurance and private) made for a particular day or time frame.
Immunizations Report → will show all the past immunizations given to a patient or a group of patients within a defined date range.
Previous Diagnosis → will depict all the diagnosis codes that have been used in the past for any given patient.
Recall Preview Report → will list accounts that meet the recall parameters selected, but do not have appointments matching the appointment parameters selected.
Patient Balance → will list patients with a patient account balance.
Aged Receivables
Aged Receivables → provides a listing of accounts, showing the balances in aging buckets.
Aged Receivables (Credit) → provides a listing of accounts, showing the credits in aging buckets.
Analysis
Control Totals → shows Total Credits and Total Debits in each Control.
Referring Physician by Rank → will “rank” referring providers to display providers, in order, that referred the most patients.
Practice Financial Analysis → analyzes a practice’s revenue for any specified month end period and will provide a trending that can be tracked from month to month and year to year.
Service Provider Visit Report → used to quickly see the number of visits for a selected timeframe broken down by service provider.
Procedure Analysis → will break down each CPT code by the description, total number of units, charge amounts, insurance payments, private payments and adjustments.
Payment Analysis → shows each account in the selected Account Category that has payment transactions in the (Payment Entry) date range.
Net A/R & Revenue → will reflect anticipated collectible revenue for charges during specified periods based on the primary insurance filing of that charge and the insurance plan’s related fee schedule expected amounts.
Appointment Scheduling
Missing Visit Report → will look for patient accounts that have appointments that meet the appointment filter criteria, but do not have charges entered that match the Date range.
Expected Collections Report → creates a list of patients based on appointment criteria and shows the expected dollar amount to collect from those patients.
Referral Review → provides the practice with a list of patients that have an insurance plan on their account that is flagged as a managed care plan or referral required, but do not have a current open referral.
Appointment List → will print the appointment schedule for a specified date, location, resource, appointment resource, or appointment status.
Appointment Wait List → will print a list of patients on the appointment scheduler wait list.
Collections
Collection Incident Activity → lists Collection Incidents that match the criteria specified by the use.
Collection Aged Receivables → shows the aging of balances in Collection Incidents, and is grouped by Collector.
Promise to Pay Analysis → will show patients that have a current promise to pay as well as patients who have missed their payments.
Collector Analysis → will track the progress of each Collector, their Account Assignments, Amount Collected and Commission for the date range entered.
Delinquent
Delinquent Transactions → will assist the user in identifying transactions they deem as past due and reporting those transactions for review.
Electronic Claims
X12837 V5010 Electronic Claims Module → creates the Electronic Claim File for a filing on a certain date. We do not recommend end users running this report as it will create a claim file for claims already created and if transmitted will cause duplicate claims.
Insurance
HCFA 1500 → will regenerate paper claims based on the Transaction Start and End date selected.
Insurance Filing → shows all accounts that have had a claim generated for them during the selected process.
Insurance Reimbursement by Procedure → analyzes CPT codes that were billed during a selected time frame.
UB-04 HCFA 1450 → will regenerate UBs for the selected time frame.
Primary Insurance Payor Mix → will group Primary Insurance Payors by Enterprise, Resource or Financial Location.
Remittance → will generate individual EOBs for a patient that has had a claim paid/adjusted on an ERA, and see the information that was sent back from the carriers.
Unprocessable Claims → will show claims with claim rules that have not been met.
Revenue & Service
Revenue and Service by Control → will show Revenue and Service for a specified Date range by Control.
Revenue and Service by Transaction → will show Revenue and Service for a specified Date range by Transaction.
Revenue and Service by CPT Group → will show Revenue and Service for a specified Date range by CPT Group. (Includes reversals)
Revenue and Service Analysis → will show Revenue and Service for a specified Date range. (Does not include reversals)
Tables
Account Category → will provide the user with a listing of all existing Category names, and codes and the Billing Default that is attached to each.
Insurance Plan → will provide the user with a listing of all existing plan names, plan codes, address and phone numbers for each plan.
Fee Schedules → will give you a breakdown listing of all Fee Schedules set up in your database.
Resource Provider → will give you a detailed listing of all Providers set up in your database.
Referring Physician → will give you a detailed listing of all Referring Providers set up in your database.
Appointment Category → will give you a listing of all Appointment Categories set up in your database.
Diagnosis Codes → will give you a listing of all Diagnosis Codes set up in your database.
Employers → will give you a listing of all Employers set up in your database.
Locations → will give you a detailed listing of all Locations set up in your database.
Adjustments → will give you a listing of all Adjustment Codes set up in your database.
Payment Codes → will give you a listing of all Payment Codes set up in your database.
Insurance Category → will give you a detailed listing of all Insurance Categories set up in your database.
Appointment Reasons →will provide the user with a listing of all Appointment Reasons in the system, and if entered, the time required for each appointment reason.
Diagnosis Groups → will give you a listing of all Diagnosis Groups set up in your database.
Physician Specialties → will provide a list of all specialties that are set up in your database.
Schools → will give you a listing of schools set up in your database.
Zip Code → will give you a listing of cities, states and zip codes set up in your database.
CPT Groups → will list all CPT groups established in the system.
Account Billing → will provide the code associated with each Account Billing description, the type of statement assigned to the visit bill type and the auto-change bill type.
Provider Numbers → will show the location each provider is attached to, as well as all numbers associated with the providers.
Account Source →will give you a listing of the different sources established in the system with the codes associated with the source name.
Account Status → will show the code, name of status, status type and whether it is part of collections.
Installed Media → shows all reports in the system, their version number, the date they were created and the date they were last modified, as well as if there are any special security requirements necessary to run the report.
User Security Rights → will list individual users and the rights assigned to them.
Claim Rules → will show you rules that are active/inactive and the insurance plan/category they are attached to.
Transaction Journal
Transaction Journal By Control → will show charges, payments and adjustments by Control for a specified data range.
Transaction Journal By Provider → will show charges, payments and adjustments by Provider for a specified data range.
Transaction Summary by Control → will show charges, payments and adjustments by Control with providers broken out in each control for a specified data range.
Daily Account Journal → will show charges, payments and adjustments by Control for a specified date.
Open Control Transaction Audit → will show charges, payments and adjustments in open controls.
On Hold Transactions → will allow you to see any charges within an account that are currently “on hold”.
Revenue Journal → provides detailed information regarding the collection of payments as applied to the corresponding dates of service.
Transaction Credit Balance → will allow the user to identify any account with transaction credits.
Top Reports Ran in MedEvolve
Transaction Journal by Provider
Transaction Journal by Control
Unprocessable Claims
Insurance Filing
Aged Receivables
Practice Financial Analysis
Appointment List
Procedure Analysis
Revenue and Service Analysis
Revenue and Service by Control
Revenue and Service by CPT
Revenue and Service by Transaction
Revenue Journal
Control Totals
