How can I avoid sending a Corrected Claim to a payer
Corrected Claims should not be sent for a payer
A user may see messages like the following within Practice Insight from a payer that does not allow corrected claim submissions.
- Carrier does not allow corrected claims. Remove ICN field information and change claim frequency to 1. Or
- Medi-Cal does not accept Voids or Adjustments electronically (Claim Frequency must = 1 in electronic claims)
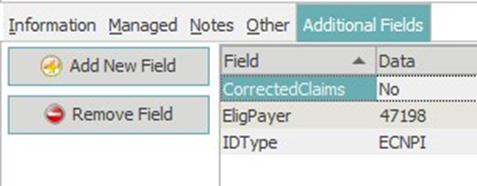
A setup within the Insurance Plan can be set to where all claims submitted to the carrier are submitted with the claim frequency of 1 (Original Claim). Within the Insurance Plan open the Additional Fields tab and select Add New Field. Add the field CorrectedClaims and then place No under the Data column field.
Note: Medicare does not accept corrected claims. Medevolve does not create corrected claims to Medicare payers. Please contact local Medicare plan for proper procedure of submitting a corrected claim or appeal claims.
